Data Analytics and AI for Healthcare
As more and more information becomes digitized throughout patient care, the healthcare industry faces challenges and opportunities in its approach to data analytics. Global health organizations and insurance companies must make faster data-driven decisions to improve the quality of care and contain costs while addressing modernization efforts and regulatory requirements.
The Altair® RapidMiner® data analytics and artificial intelligence (AI) platform reduces healthcare IT complexities and streamlines areas like claims and reimbursement processing, interoperability, patient adherence and satisfaction analysis, physician performance analysis, and revenue cycle management. Our healthcare analytics solutions empower organizations to transform their data – resulting in cost savings, better patient care, and better decision-making.

Machine Learning and AI for Healthcare Analytics
Altair’s low- and no-code machine learning and AI solutions help users easily generate and share insights derived from financial, administrative, operational, and clinical data to reduce risk and improve the quality of care. It also helps teams make confident data-driven decisions and understand how models make predictions and arrive at outcomes. Transparency in the model building process and explainable AI improves data governance.
With Altair’s tools, organizations can:
- Drive better outcomes for patients and foster regulatory and reimbursement efficiencies.
- Pinpoint predictive behaviors to manage long-term costs, spur revenue growth, foster effective communication, solve complex business problems, and improve therapeutic adherence.
- Predict how often patients will require medical attention, identify patients at risk for readmittance, and develop strategies to reduce unnecessary, expensive urgent care/emergency visits for patients.
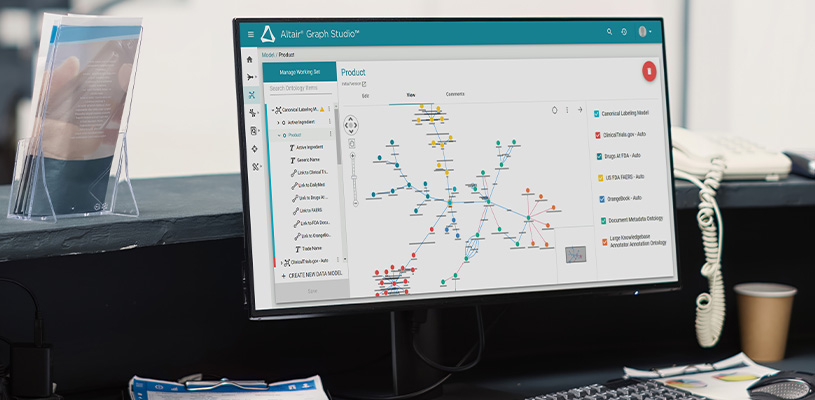
Knowledge Graphs for Next-Level Healthcare Analytics
With Altair RapidMiner’s knowledge graph solutions, organizations can apply a semantic layer atop their data estate to identify otherwise hidden patterns. Insurance providers can leverage data to ensure patient considerations are met without compromising care. Organizations can track data from its inception to its use in the decision-making process.
Moreover, knowledge graphs help teams:
- Identify relationships in data.
- Align product and policy development to match customer needs and reduce churn.
- Identify suspicious patterns and anomalies to detect fraud and minimize losses.

A Flexible, Modern SAS Language Environment
With strict regulatory requirements governing vital personal patient data, organizations require a secure, interoperable environment to process that data. Organizations can migrate to Altair’s flexible, reliable SAS language environment without losing time converting code before or during deployment. The solution boasts an intuitive, familiar user experience that blends SAS language compatibility with the benefits of a modern, interoperable system that can compile scripts in R and Python.
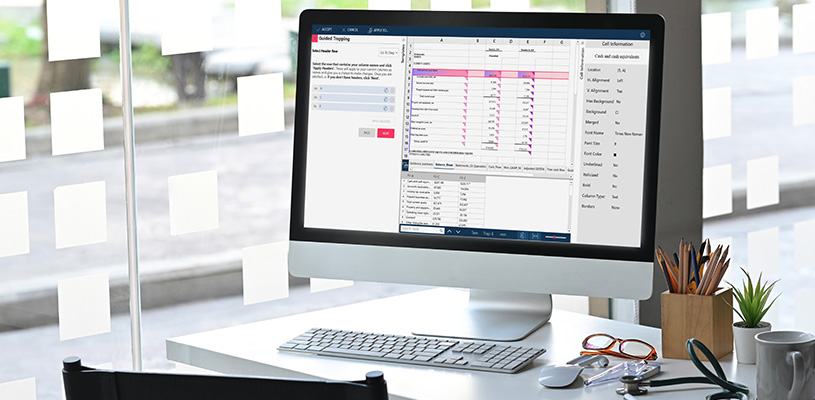
Data Preparation for Healthcare Analytics
Altair empowers healthcare organizations to access, cleanse, and transform data—helping break down data silos. Organizations can build automated workflows for standardized, shareable assets that optimize strategic planning, streamline operations, and maximize resources while controlling cost.
In addition, they can:
- Automatically reconcile disparate reporting formats such as the Excel, PDF, unstructured, and semistructured files needed to achieve regulatory compliance.
- Reduce repetitive, manual effort with seamless automated workflows.
- Easily merge electronic medical records (EMR), demographic, clinical, primary market research, and other disparate patient data sources.
- Track resources to anticipate need and deploy rapid, targeted responses.
- Evaluate new patient data to ensure accurate claims reporting.
The Impact of the AI Fabric
Inaccessible data hosted in siloed and proprietary financial systems – and in remittance files such as U.S.-based 835 transaction files, claims paperwork, and third-party payment information – complicates revenue cycle management. Altair RapidMiner automates repetitive, error-prone processes associated with accessing and reconciling financial healthcare data, eliminating manual work and accelerating the revenue cycle.
For Providers and Health Systems
- Streamline finances, reporting, outbound claims, and inbound remittances.
- Automate manual, error-prone workflows to rapidly process disparate data sources into a shareable asset for organizations from large healthcare systems to small private practices.
- Anticipate and scale resource and utilization needs (like the number of beds and staffing) with predictive analytics and machine learning.
- Identify and target at-risk patient populations with proactive outreach to reduce costly ER visits and readmission.
For Insurers and Payers
- Access to wide-ranging data to build a patient 360 model for all members.
- Optimize strategies to manage cost and risk while improving value and patient care.
- Collate and transform volumes of clinical, demographic, and operational data for insurers. Prepare for market disruptions like regulatory and reimbursement changes while comparing benefit schedules.
- Payers can use predictive modeling to follow patient trends and anticipate cost adjustments.