Healthcare and Life Sciences
Altair helps pharmaceutical, biotech, and medical device companies develop and produce better products in less time, improve patient outcomes, and reduce costs. Our simulation, data analytics, artificial intelligence (AI), and high-performance computing (HPC) solutions help healthcare industry teams understand complex issues, unlock medical breakthroughs, and bring the latest advancements to market faster while ensuring efficacy and safety.
Healthcare and Life Sciences
Altair helps pharmaceutical, biotech, and medical device companies develop and produce better products in less time, improve patient outcomes, and reduce costs. Our simulation, data analytics, artificial intelligence (AI), and high-performance computing (HPC) solutions help healthcare industry teams understand complex issues, unlock medical breakthroughs, and bring the latest advancements to market faster while ensuring efficacy and safety.
Healthcare and Life Sciences
Altair helps pharmaceutical, biotech, and medical device companies develop and produce better products in less time, improve patient outcomes, and reduce costs. Our simulation, data analytics, artificial intelligence (AI), and high-performance computing (HPC) solutions help healthcare industry teams understand complex issues, unlock medical breakthroughs, and bring the latest advancements to market faster while ensuring efficacy and safety.
Accelerate Drug Discovery, Development, and Manufacturing
Use the Altair® RapidMiner® platform to build knowledge graphs that combine and analyze data stored in a wide variety of formats – including SQL databases, big data repositories, and spreadsheets – along with unstructured sources like drug labels, case narratives, medical histories, journal articles, research papers, and business vocabularies, including the Medical Dictionary for Regulatory Activities (MedDRA), WHODrug Global, EMA EudraVigilance, and the FDA Adverse Event Reporting System (FAERS).
Create AI models to streamline patient recruitment and support regulatory compliance reporting workflows, increase the efficiency of safety reporting, improve data exchanges between R&D and manufacturing operations, and create synthetic control arms using real world data. Use our fully validated, flexible alternative SAS language environment as a component of your statistical computing environment (SCE) for the analysis and reporting of clinical data.
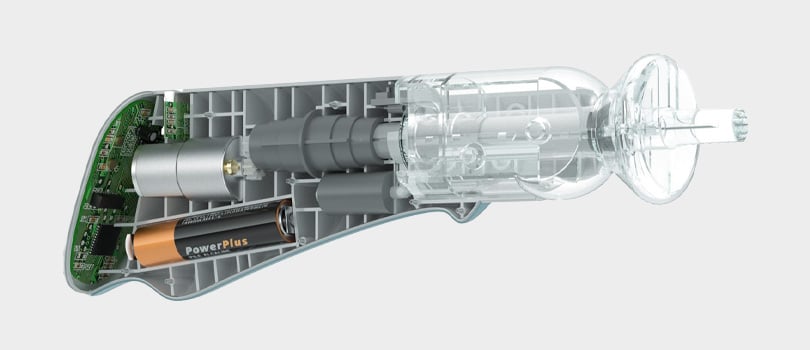
Design and Build Robust, Cost-Effective Medical Devices
Use the Altair® HyperWorks® platform to design medical and wellness devices that balance cost, weight, manufacturability, reliability, and performance. Deliver devices and equipment that can withstand the punishment of everyday use, sterilization, and even misuse. Ensure first-time right application-specific integrated circuit (ASIC) designs with our silicon debugging and digital simulation solutions. Employ a multiphysics approach early in the design process to optimize component and system structural, thermal, electrical, and electromagnetic performance and size requirements.
Learn how Johnson & Johnson uses Altair HPC tools to speed vaccine development.
Read Story
Expedite Clinical Trials
Clinical trials are crucial in drug and medical device development, but they’re also expensive and time-consuming. Clients use Altair’s AI and data analytics software to optimize trial design by identifying suitable patient populations, predicting outcomes, and monitoring trial progress in real time.
Design Robust Implants and Prosthetics
Altair solutions empower organizations to develop medical products for strength, longevity, tissue compatibility, and patient comfort. These tools enable the modeling, analysis, and optimization of complex biological and orthopedic structures. Our optimization technology simulates mechanical stress influence on bone growth and load distribution to prevent implant failures, while our modeling and visualization technology is tailored for creating patient-specific prosthetic designs.
Altair’s simulation-driven design approach delivers an unparalleled user experience, seamlessly integrating geometry creation, design verification, optimization, and manufacturability within one environment. Leveraging generative design, topology optimization, motion simulation, and robust implicit modeling, users can rapidly generate complex, 3D-printed lattice structures ideal for osseointegration and vascularization. The integrated meshless solver accelerates analysis of medical equipment and patient-specific implants, facilitating evaluation of complex lattice and trabecular structures. Customizable scripting adapts the solution to diverse design challenges. By closing the loop between simulation and design, Altair empowers engineers to create superior implant designs.
How can we help you develop the next medical innovation?
Contact Us
Make AI Integral to Drug Development and Personalized Medicine
Pharmaceutical researchers use generative AI to discover and develop revolutionary drugs faster and more economically than traditional methods. AI also plays a major role in precision medicine design and personalized medicine when used by medical professionals to analyze a patient’s genome, identify biomarkers, and predict how a patient is likely to react to, metabolize, and benefit from a drug.

Expand the Drug Pipeline with HPC
Customers depend on Altair® HPCWorks® to optimize complex HPC environments and accelerate mission-critical healthcare and life sciences research. Whether on premises, in the cloud, or in hybrid environments, Altair's trusted workload management tools – along with solutions for HPC admin control, user access, pinpointing I/O bottlenecks, and more – provide scalability and efficiency that lowers the cost of drug development and increases the likelihood of success at every stage, from preliminary molecular studies to processing clinical trial data.

Optimize Pharmaceutical Supply Chains
Use Altair’s machine learning software to predict potential disruptions, identify alternative suppliers, minimize risk, optimize inventory levels, and reduce waste. AI models built in SAS, Python, or R — or produced using our intuitive visual workflow designers — can monitor data from every step in the supply chain to ensure inputs meet your quality standards and prevent spoilage. Build dashboards to monitor orders, shipments, and supplier pricing in real time. Avoid stockouts and overstocking by anticipating demand based on market trends, seasonal variations, and even social media sentiment.

Improve Drug Manufacturing Processes
Altair’s discrete element modeling (DEM) solution simulates the behavior of particulate materials used in drug production, from excipients to tablets and capsules. Accurately simulate particle behavior to optimize critical manufacturing processes such as mixing, coating, granulation, hopper discharge, and tableting. By providing predictive insights into process performance and product quality, users can accelerate development, reduce costs, and minimize physical testing.
Altair’s integrated multiphysics simulation and AI solutions accelerate pharmaceutical development and manufacturing. By simulating complex particle-fluid systems and generating synthetic data for predictive digital twins, we optimize processes, reduce costs, and ensure product quality and compliance.
Featured Resources
Revolutionizing Oral Healthcare: Exploring the Fusion of Digital Twin Technology with Data Analytics and Altair Radioss
Presentation by Dr. Jingchao Sun, R&D Senior Director at iLittleMiracle as part of Altair's Future.Industry 2024 conference.
Nowadays, orthodontists need to utilize digital tools to develop appropriate treatment plans for patients. Under the existing traditional techniques, it is difficult to predict the forces within the oral cavity and can only observe the outcomes. Clearly, this imposes numerous constraints on orthodontists. iLittleMiracle(iLM), however, employs the Altair Radioss solver to offer biomechanical simulations for each kid's every treatment stage, enabling orthodontists to analyze and anticipate the forces within the oral cavity. Consequently, orthodontists can combine their clinical experience and choose more rational treatment plans. Building upon this foundation, RomuTech utilizes the Radioss simulation results as an effective training dataset for data analytics machine learning. By integrating the advantages of high precision and efficient predictability, iLM provides orthodontists with reliable, efficient, and visualized digital tools. This marks the first application of digital twin technology in the field of dentistry, addressing industry pain points and leading the way into a new era of digital delivery.

Tracking Virus Variants with AI – Argonne National Laboratory Researchers Win Gordon Bell Special Prize
The COVID-19 pandemic has impacted the entire planet, and researchers continue to investigate its catalyst: the SARS-CoV-2 virus and its variants. Discovering variants of concern (VOCs) quickly can save lives by giving scientists time to develop effective vaccines and treatments — but existing variant-tracking methods can be slow. A team of researchers at Argonne National Laboratory, along with university and industry collaborators, tackled the problem of tracking virus variants by using artificial intelligence (AI). The powerful Polaris supercomputer at the Argonne Leadership Computing Facility (ALCF), which is enabling science in the runup to the Aurora exascale system, enabled the research with help from Cerebras' AI-hardware accelerator and NVIDIA's GPU-accelerated Selene system. Polaris is equipped with GPUs and with workload orchestration by Altair® PBS Professional®. The project team won the ACM's prestigious 2022 Gordon Bell Special Prize for High Performance Computing-Based COVID-19 Research. The results the Argonne researchers and their collaborators have achieved paves the way for faster, more detailed insight into the virus mutation process, enabling scientists to act on emergent variants and develop ammunition to reduce severity and slow the spread, ultimately saving lives.

Medtronic Reduces Medical Stent Stress by 71%
Medtronic designs and manufacturers medical devices used the world over. Traditionally, computer aided engineering (CAE) and virtual simulation were not fully utilized within the industry as the verification process for often microscopic components was too slow. When designing a new medical stent (an expandable mesh inserted into a patient's artery to keep it open) Medtronic wanted to improve the design and speed up the validation process. Altair ProductDesign worked closely with Medtronic’s own engineers to optimize the performance of the new stent.

Digital Twins of Oral Solid Dose (OSD) Manufacturing Processes
The use of digital twins for virtual process optimization is a key component of the digital transformation strategy in the pharmaceutical industry, but their development and deployment require the combined use of a wide range of technologies such as physics-based simulation, machine learning, high-performance computing, real-time dashboarding and IoT. Altair is uniquely positioned to deliver an end-to-end solution in this context.